impact testing measuring depression in elderly with tbi|A systematic review of mood and depression measures in people : wholesaling Traumatic brain injury usually results from a violent blow or jolt to the head or body. An object that goes through brain tissue, such as a bullet or shattered piece of skull, also can cause traumatic brain injury. Mild . WEB29 de abr. de 2023 · Pelo Clube do Povo, o atleta receberá um salário de 1,4 milhão de reais – o valor inclui luvas diluídas pelo acerto com o atacante, podendo ser utilizado .
{plog:ftitle_list}
WEB14 de nov. de 2023 · Padaria Ideal Olaria Cinco Bocas, #4530 among Rio de Janeiro restaurants: 237 reviews by visitors and 19 detailed photos. Find on the map and call to .
Apathy and depression are both common after moderate to severe traumatic brain injury (TBI) and may be especially important to distinguish in older adults with TBI. The authors examined apathy and depression in relation to cognitive performance domains and .
To increase the likelihood of patients being offered proportional and appropriate treatment, it would be useful to clarify which mood assessment measures are valid for use . Traumatic brain injury usually results from a violent blow or jolt to the head or body. An object that goes through brain tissue, such as a bullet or shattered piece of skull, also can cause traumatic brain injury. Mild .When assessed shortly after traumatic injury, rates of depression range from 8–60%. 51, 74, 100 However, among long-term follow-up studies that exist, rates of depression range between 9–31% at 6–12 months post-injury. 51, 95 However, studies have reported higher rates of depression in those who have concomitant traumatic brain injury . Traumatic brain injury’s (TBI) after-effects can show up months and years after a long-forgotten head injury from a car accident, a fall, sport-related head injury, etc. . Often overlooked in .
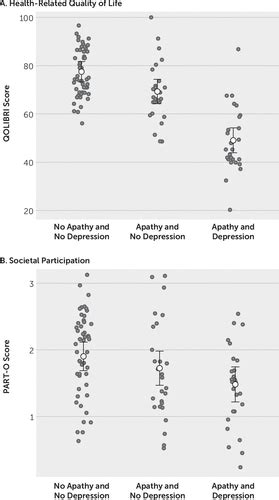
Objective: Apathy and depression are both common after moderate to severe traumatic brain injury (TBI) and may be especially important to distinguish in older adults with TBI. The authors examined apathy and depression in relation to cognitive performance domains and their potentially unique contribution to psychosocial functioning in this patient population. . Goal Examples; Characterize cognitive and behavioral function: Establish cognitive baseline before or after illness, injury, or treatment: Evaluate the impact of a medical issue on cognitive .Study selection. Searches were conducted in PubMed, CINAHL, PsycINFO, ProQuest, of Science, and Google Scholar. The specific search terms used were “depression,” “major depression,” “major depressive disorder,” “traumatic brain injury,” and “brain injury,” as well as the names of instruments commonly used to measure symptoms of depression.
Apathy and Depression Among People Aging With Traumatic
The Geriatric Depression Scale (GDS) is specifically designed to screen and measure depression in older adults. It contains 30 forced-choice “yes” or “no” questions, a format that is helpful for individuals with cognitive dysfunction. Questions relate to how an individual has felt in a specified time frame. Psychiatric disorders frequently occur following a traumatic brain injury (TBI) and depression is the most common.1,2 When psychiatric diagnostic criteria are used, the prevalence of major depressive episode (MDE) in persons with moderate to severe TBI ranges from 26–36%.3–7 A recent study in the Journal Of the American Medical Association suggests that . Another definition that can help to characterize TBI comes from The Demographics and Clinical Assessment Working Group of the International and Interagency Initiative Toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health; it states that “a traumatic brain injury is an alteration in brain function, or . Mortality rates after brain injury are highest in people with a severe TBI. In the first year after a TBI, people who survive are more likely to die from seizures, septicemia, pneumonia, digestive conditions, and all external causes of injury than are other people of similar age, sex, and race. [] However, the mortality rate after severe TBI has decreased since the .
The Centers for Disease Control and Prevention has termed traumatic brain injury (TBI) the “silent epidemic,” 1 and within this silent epidemic, there is a seemingly silent population: older adults with TBI. Older age is a variable known to negatively influence outcome after TBI, 2 – 4 but analyses illuminating why this is the case, as well as information regarding age-appropriate .
The exam may include a blood test measuring two biomarkers in the blood, which, when elevated, can indicate a brain injury. Biomarker tests, including a new one that was approved by the Food and Drug Administration in 2023, could help doctors sort out a TBI in older adults from other preexisting conditions, Gardner says.Traumatic brain injury (TBI) is a form of nondegenerative acquired brain injury, resulting from an external physical force to the head (e.g., fall) or other mechanisms of displacement of the brain within the skull (e.g., blast injuries). Consistent with the diagnostic criteria detailed in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric .Fann, J.R., Hart, T., Schomer, K.G.. Treatment for Depression after Traumatic Brain Injury: A Systematic Review. Journal of Neurotrauma 26:2383-2402, 2009. Authorship. Depression after Traumatic Brain Injury was developed by Jesse Fann, MD, MPH, and Tessa Hart, PhD, in collaboration with the Model Systems Knowledge Translation Center. Figure 3.Odds ratio (OR) of depression over time post mild traumatic brain injury (mTBI) (A) and age at injury (B).(A) Data were stratified into early phase (6 months−1 year post-mTBI), late-early phase (1–2 years .
In 2007, Wilde et al. examined the impact of co-morbid Obstructive Sleep Apnea (OSA) diagnosed after the TBI on the cognitive functioning of patients with TBI, in comparison to patients with TBI but without OSA. Those with TBI with OSA performed significantly worse on verbal and visual delayed recall measures and had more attention lapses than .Traumatic brain injury (TBI) happens when a sudden, external, physical assault damages the brain. . It is one of the most common causes of disability and death in adults. TBI is a broad term that describes a vast array of injuries that . There are numerous post-TBI self-report symptom inventories available to record subjective symptoms and the degree of impact or level of severity each endorsed symptom is having on an individual (e.g., Rivermead Post Concussion Symptoms Checklist [], Concussion Signs and Symptoms Checklist).Residual signs and symptoms of sport-related concussion .
Importance Cognitive dysfunction is common after traumatic brain injury (TBI), with a well-established dose-response relationship between TBI severity and likelihood or magnitude of persistent cognitive impairment. However, patterns of cognitive dysfunction in the long-term (eg, 6-month) recovery period are less well known. Objective To characterize the .The CSDD is specifically designed to measure depression in persons with dementia. 20-30 mins . 60-64, 65-74 and 75-84. Used in patients with stroke, dementia, traumatic brain injury, major psychiatric disorders and substance abuse. Author and year: . Useful in assessing the impact of anxiety upon on older person's life and ability to .Three patients each present with cognitive complaints following a history of mild traumatic brain injury (mTBI). Patient 1 is a successful 45-year-old financial advisor with a large client base. He reports that 3 months following a rock climbing accident he can’t do his job anymore. He says, “I can’t think straight.” Patient 2 is a 78-year-old independent-living woman who has
Abstract. During the last 30 years, there has been a substantial increase in the study of posttraumatic stress disorder (PTSD). Several high-profile traumatic events, such as the wars in Afghanistan and Iraq, and the terrorist attacks of September 11 on the World Trade Center, have led to a greater public interest in the risk and protective factors for PTSD.in up to 77% of people with TBI (2). Depression post-TBI has been associated with extensive adverse outcomes such as impaired psychosocial function-ing, impaired cognitive performance, and increased risk of other psychiatric disorders, such as anxiety disorders (3). It is also more common for those with post-TBI depression toTRAUMATIC BRAIN INJURY (TBI) has been defined by the Centers for Disease Control and Prevention (CDC) as “a bump, blow or jolt to the head that disrupts the normal function of the brain” that can result from external force to the head, including whiplash, blast exposure, or penetrating injury. 1 There are 2 critical elements of this definition: (1) a blow to the head, .
Background Mild traumatic brain injury (mTBI) is an increasing public health problem, because of its persistent symptoms and several functional consequences. Understanding the prognosis of a condition is an important component of clinical decision-making and can help to guide the prevention of persistent symptoms following mTBI. The prognosis of . Traumatic brain injury (TBI) is a global public health concern and one of the leading causes of death and disability, with an estimated 64–74 million persons sustaining a TBI each year. 1 TBI is traditionally identified as mild, moderate, or severe at the time of injury by a measure called the Glasgow Coma Scale (GCS). Although most of the literature on the .Traumatic Brain Injury (TBI) - Etiology, pathophysiology, symptoms, . Acceleration or deceleration can injure tissue at the point of impact (coup), at its opposite pole (contrecoup), or diffusely; the frontal and temporal lobes are particularly vulnerable to this type of injury. . In the United States, adults with severe traumatic brain .
A systematic review of mood and depression measures in people
dampness tester
{{public.contentView.content.bsid}} · Sincronizado em {{public.
impact testing measuring depression in elderly with tbi|A systematic review of mood and depression measures in people